Pharmacy First Service
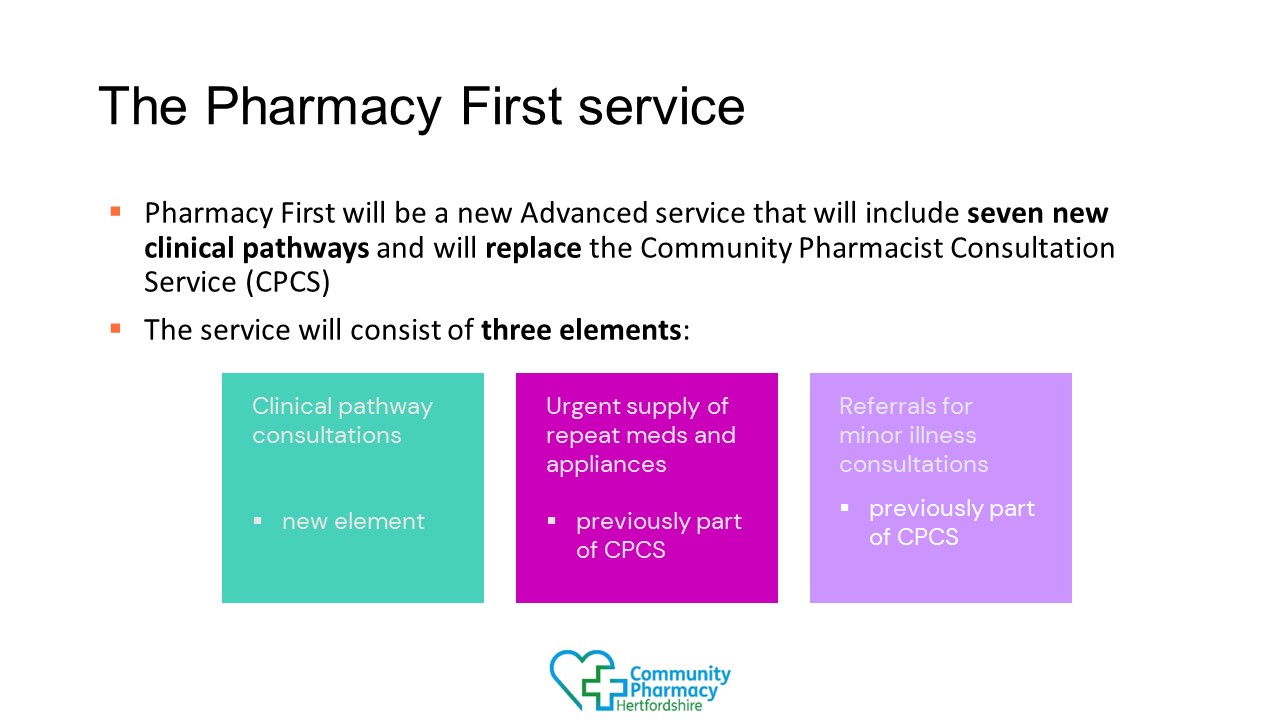
The new Pharmacy First service, which was announced as part of an an agreement setting out how the £645 million investment pledged within the Delivery plan for recovering access to primary care will be used to support community pharmacy services.
The Pharmacy First service, commences on 31 January 2024.
The introduction of a national Pharmacy First service alongside expansions of contraception and blood pressure checking services are an important step forward for community pharmacies and their patients, but this development this will not solve all of the problems that pharmacies are struggling with. Community pharmacies remain under significant financial and operational pressure with businesses of all sizes reporting record losses. While these new services will offer some extra funding, this will not address the underlying funding deficit in the sector, and finding the capacity to deliver them will be a real challenge
Full information on the Pharmacy First service including FAQs is available via the CPE website.
View pharmacies in Hertfordshire and West Essex registered to provide the Pharmacy First Service. (updated 22.4.24)
A video (10 minutes) for Pharmacy First with key messages from CPH Chief Officer, Helen Musson, is available to help you get started:
CPH Pharmacy First Video (This is currently undergoing an update and a new version will be uploaded to the website shortly – please contact info@cpherts.org.uk for further information)
The slides with the resources links are available to access:
CPH Pharmacy First 22 January 2024
Please communicate with your Community Pharmacy PCN Integration Lead when you will be ready to provide the Pharmacy First service or any challenges to delivery. Contact details of your PCN lead for your pharmacy is on the HWE ICB website.
Videos talking pharmacists through each of the clinical pathways in preparation for the service are on the CPE website.
Hertfordshire and West Essex (HWE) Integrated Care Board (ICB) is keen to support community pharmacists locally to deliver the new Pharmacy First service. The HWE ICB Training Hub provided local training to 80 pharmacists on Sunday 21 January and has made available further training outlined below to pharmacists working within Hertfordshire and West Essex. Booking details have been shared by email.
ONLINE PHARMACY FIRST TRAINING
Online e-learning is available through ECG Training (https://ecgtraining.co.uk/) that is standalone and does not include otoscope training. Please do not book on to this course if you are looking for the e-learning and otoscope training combined.
COMBINED PHARMACY FIRST TRAINING (ONLINE AND IN PERSON OTOSCOPE TRAINING)
New dates of blended training are available (online and in person otoscope training). Full information with booking details will be sent out by email. The online e-learning modules are released soon after a booking place is confirmed.
As a reminder HWE ICB has partnered with ECG Training (https://ecgtraining.co.uk/) to offer a Pharmacy First course in a blended format, divided into two segments:
- online e-learning modules (completion before in person training); topics covered outlined below
- in person training, which concentrates on the practical utilisation of the otoscope.
Tuesday 6 February (venue to be confirmed)
- 19:45 – 21.30 (10 places available)
Sunday 11 February (venue to be confirmed) AND
Sunday 18 February (venue to be confirmed)
with availability for 80 delegates on each day for the following timeslots:
- 09:00 – 10:45 (20 places available)
- 11:00 – 12:45 (20 places available)
- 13:15 – 15:00 (20 places available)
- 15:15 – 17:00 (20 places available)
The online eLearning component covers a variety of essential topics as listed below:
| Type of Course | Content | Specifics | Included |
| Online Training Course |
|
|
|
The following four IT suppliers are currently working with NHS England to develop their systems to include functionality to support the service, further suppliers are expected to be added to this list so please check the CPE website (under the section “Getting ready to provide the service”) for further updates:
| System and supplier |
| HxConsult (Positive Solutions) |
| Pharmacy Manager (Cegedim) |
| PharmOutcomes (Pinnacle Health) |
| Sonar health (Sonar informatics) |
Month
Minimum number of clinical pathways consultations
February 2024
1
March 2024
5
April 2024
5
May 2024
10
June 2024
10
July 2024
10
August 2024
20
September 2024
20
October 2024 onwards
30
If you were unable to attend the latest Pharmacy First webinar series please see below a link to all current recorded webinars:
CPE have also provided a live webpage to keep you up to date with important dates CPCF services and Terms of Service – important dates
- Community pharmacy advanced service specification: NHS Pharmacy First Service – includes PGDs
- Pharmacy First – Medicines list for clinical pathway consultations
- CPE Pharmacy owner checklist: getting going with the Pharmacy First service
- CPE Pharmacist checklist: getting going with the Pharmacy First service
- CPPE Pharmacy First self-assessment framework
- Pharmacy First PGD and Protocol Authorisation sheet
- Pharmacy First Webinars explaining full details of the service
- CPE website
- CPE drop in sessions and additional resources
- CPH website
- Resources to promote the service
Training Support Please note this information is not endorsed by CPH.
CPPE Pharmacy First Information and Support:
https://www.cppe.ac.uk/services/pharmacy-first/
Cliniskills training (NHS England funded) for Pharmacy First, including otoscope training webinar on 18th Jan 2024:
https://www.cliniskills.com/community-pharmacists/
Pharmacy Magazine has useful information including a section on Pharmacy First, news articles and training modules to help you stay up to date and is free to sign up:
https://www.pharmacymagazine.co.uk
Agilio’s free Courses for Pharmacists has been developed to support the rollout of the NHS Pharmacy First Service that includes 7 e-learning courses available on the iLearn platform for these common conditions. These accredited courses are based on NICE CKS and aligned to the NHS England clinical pathways and PGDs. All these courses are free to access and include a case study and multiple-choice questions to test understanding, with a certificate of completion:
https://cpherts.org.uk/wp-content/uploads/sites/66/2024/01/Pharmacy-First-Agilio-Software-003.pdf
Campaign and promotional materials are now available, please visit the CPE website.
Where can I find information about training to support me? Information is available above as to known training availability that can support you both locally and online. Please remember that there is no mandatory training and that the requirements of the service are as follows:
- The pharmacy owner must ensure that pharmacists providing the service are competent to do so, including the use of an otoscope (except for DSPs) and be familiar with the clinical pathways, clinical protocol and PGDs. This may involve completion of training.”
- “The pharmacy owner must keep documentary evidence that pharmacy staff involved in the provision of the service are competent and remain up to date with regards to the specific skills and knowledge that are appropriate to their role, and to the aspects of the service they are delivering.”
Pharmacists do not need to undertake huge amounts of training to get ready to provide the service other than to ensure that they are competent to deliver the service. The clinical pathways are very clear about red flags, safety netting and being able to refer to another provider e.g. the GP practice if they are unsure.
Do pharmacists need to complete a Declaration of Competence before providing the service? There is no requirement to complete a Declaration of Competence, but pharmacy owners must ensure pharmacists are competent to provide the service. One way for pharmacists to demonstrate they have reviewed their own competencies is by working through the Pharmacy First self-assessment framework, developed by CPPE and NHS England.
We currently get minor illness referrals from GP practices via email. Will referrals now be sent via our IT system for Pharmacy First? Initially information will be transmitted using the NHSmail functionality currently used for CPCS, but this will be enhanced in the next few weeks to provide structured data to practices (GP Connect Update Record).
When can community pharmacy NHS profiles be updated to show which pharmacies are offering Pharmacy First? When a pharmacy starts to provide the service, their Directory of Services (DoS) entries will be updated by DoS leads. As is currently the case for the Community Pharmacist Consultation Service, Pharmacy First will not be visible as a service provided by the pharmacy in NHS Profile Manager. Pharmacy profiles in NHS Service Finder will show the pharmacy as being registered to provide the service.
If a patient returns to the pharmacy i.e. 3-5 days later as per the clinical pathway after receiving an initial Pharmacy First consultation and were not dispensed antibiotics, can the pharmacist undertake another Pharmacy First consultation and dispense antibiotics if clinically indicated? Yes. The first consultation is considered closed as you provided support as required at that point in time. Pharmacists would open a second consultation with the patient and proceed as per the clinical pathway.
Can the pharmacists sign the master PGD authorisation sheet instead of each of them individually? Yes. Please note all pharmacists, including locums, providing the Pharmacy First service and hence operating under the PGDs and protocol are required to sign the PGD authorisation sheet. That also needs to be authorised by an authorising manager, who may be the pharmacy owner or a manager employed by the pharmacy owner. A copy of this completed PGD authorisation sheet should be retained by the pharmacy owner as a record of those practitioners authorised to work under the PGDs and protocol.
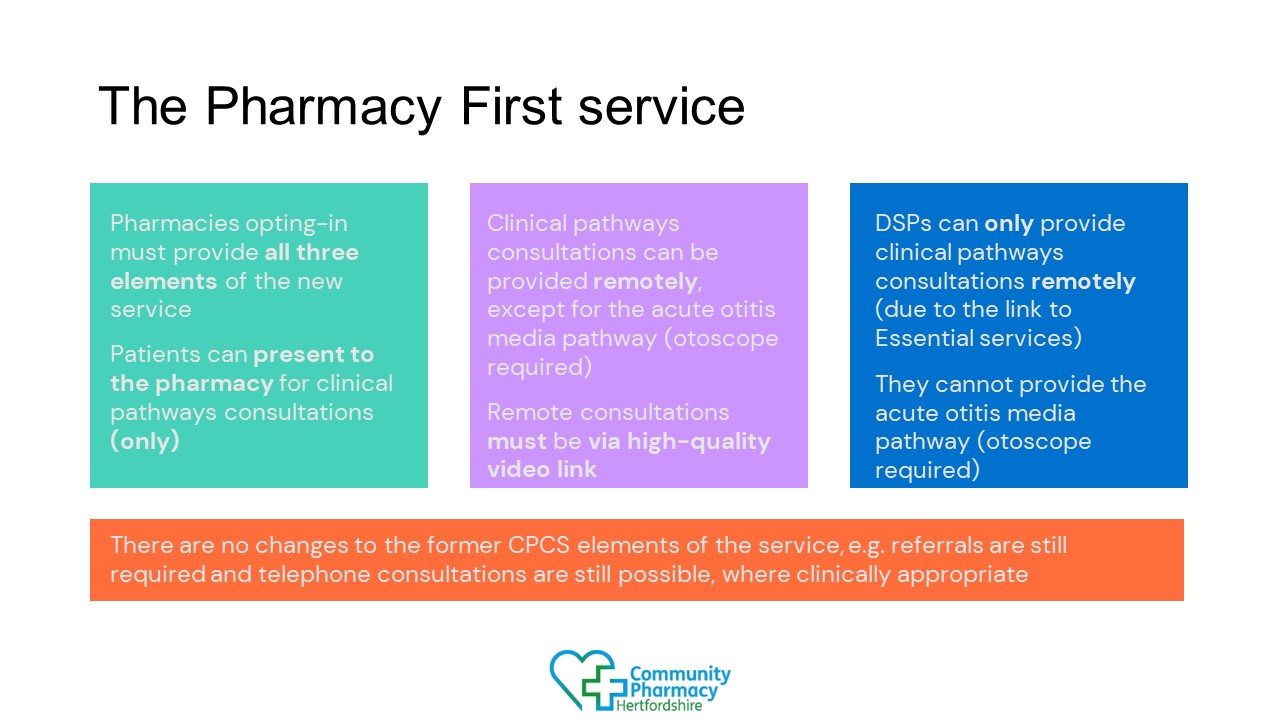
Can a pharmacy deliver one of the seven pathways for Pharmacy First by telephone? No. You can deliver consultations for six of the seven pathways remotely via live video link from the pharmacy premises and in person for the Otitis Media clinical pathway.
Can a pharmacy claim for a Pharmacy First consultation as part of the seven pathways if a patient has been supported remotely via live video link but they cannot attend the pharmacy where there is a clinical need to supply a product? No. A pharmacy would be unable to claim for a consultation if there is a clinical need to supply a product and the pharmacy cannot do so. It is appropriate to refer the patient onwards (i.e. to another pharmacy) but no fee is payable to the referring pharmacy.
If the patient passes the gateway point and the end point of the pathway for them is not to supply a medicine then this would be claimable.
Does a clinical pathways consultation i.e. one of the seven pathways referred by another provider e.g. GP practice count towards the minimum activity threshold in order to receive the monthly fixed payment and avoid the initial fixed payment being reclaimed? Yes. Please note minor illness and urgent medicines supply consultations do not count.
Could a pharmacy end up claiming two fees one for the local acuity, minor illness referral and the clinical pathways consultation referral? No. If the gateway criteria is met when the patient has been referred then the pharmacy would undertake this via the clinical pathways consultation. If the gateway is not met when the patient has been referred then the pharmacy would undertake this via the low acuity, minor illness consultation.
Please note that if the patient presents at the pharmacy and the gateway criteria is not met then the pharmacy would be expected to provide support for self care as part of the essential service provision with or without OTC supply or onward referral as appropriate. The low acuity, minor illness element of Pharmacy First can only be undertaken with a referral from another provider.
Our pharmacy is currently delivering the local UTI PGD commissioned by HWE ICB, will this continue? No. This service will be decommissioned from 29 February 2024. Pharmacies should not claim twice and follow the relevant PGD and pathway as indicated locally or nationally.
Will the pharmacy’s indemnity cover Pharmacy First? Pharmacies should check with their indemnity provider about the provision of Pharmacy First.
What happens if a pharmacy cannot provide the service at any point during its opening hours? If the service must be temporarily withdrawn by the pharmacy contractor due to circumstances beyond the scope of the business continuity plan, they must inform the NHS Directory of Services (DoS) Provider and Commissioner Helpline (0300 0200 363) as soon as possible to stop referrals being made to the pharmacy. GP practices and UEC settings within the local primary care network (PCN) must also be contacted to prevent them making further direct referrals. The pharmacy contractor must also inform the local commissioner of the service of their temporary withdrawal from the service.
Is there a timeframe in which community pharmacies have to respond to patient referrals for the Pharmacy First service? The pharmacy contractor must ensure that the service is available throughout the pharmacy’s full opening hours (i.e. core and supplementary). Where a contractor has received a referral but has not been contacted by the patient within 30 minutes of the referral, the pharmacist should consider whether they should contact the patient using the contact details set out in the referral message. The decision to contact the patient or not is for the pharmacist to make based on their clinical judgement. If the patient has not made contact before the next working day, then the pharmacist can close the referral as ‘no intervention or no supply made.’ No payment is due where there is no consultation (remotely or face-to-face) with the patient.
Visit the CPE website for more information.
NHS England have created a presentation on Update Record which contains a small amount of additional information on how filing of records will happen at general practices in the two main GP IT systems and when updates to the National Care Record Service will be sent from the GP system.
The presentation can be accessed from the CPE website.